Patient Impact
Importance of Collecting a Complete Family Cancer History
According to an expert statement issued by ASCO in February 2014, oncologists should emphasize thorough documentation of first, second and third degree cancer family history, which includes age of diagnosis, when seeing a new patient. (1)
First of Their Kind
These ASCO recommendations are the first to focus on family history capture, specifically in the field of oncology, to help determine whether they are appropriate for hereditary cancer testing. The guidelines recommend an interactive process between providers and patients, which updates the cancer family history from the initial diagnosis throughout the entire treatment and into survivorship.
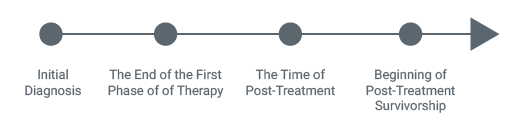
Multiple Opportunities to Reassess Cancer Family History (3)
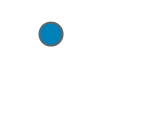
Complete Cancer Family History (2)
“After the initial visit, the ongoing relationship between the oncologist and the patient provides multiple opportunities for reassessment and updating of family history”(4)
More Education Needed
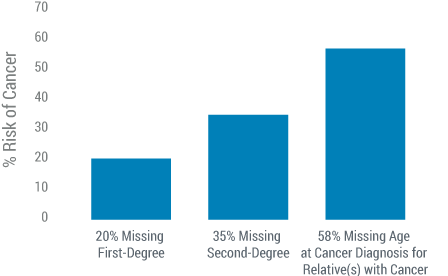
The quality of cancer family history, and referral for genetic testing among oncology practices, could be much improved, according to another ASCO special report in the Journal of Clinical Oncology by Wood, et al.(5) This study by Dr. Wood illustrated that researchers in a pilot test of quality measures, as part of ASCO’s Quality Oncology Practice Initiative (QOPI), identified low rates of complete cancer family history documentation. Dr. Wood and her colleagues looked at over 10,000 medical records of patients who had breast or colon cancer, from 212 practices. This study found that: (6)
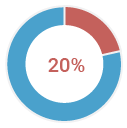
of medical charts were missing first-degree cancer family history (CFHx) information
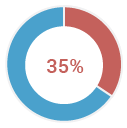
were missing second-degree CFHx information
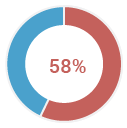
of charts were missing the age at diagnosis for relatives with cancer documented
Missing Information in Medical Charts n=10,466 (7)
Additionally, 91% of primary and specialty physicians were aware of genetic testing for breast and ovarian cancers. Only 60% of this group was aware of colorectal cancer testing. (8)
This ASCO research demonstrates the need for more education and support regarding the importance of accurate cancer family history documentation. In order to provide precision medicine and reduce the risk of misdiagnosing hereditary cancer, a proactive high-risk patient management program should be the standard for all oncologists.
An Incomplete Cancer Family History Leads To Missing A Significant Number Of Patients At Risk For Hereditary Cancer.
This was demonstrated in a recent poster presented at the 2014 ASCO annual meeting which reviewed 499 high risk family histories to determine patients’ eligibility for advanced breast or colon cancer hereditary cancer risk assessment.
Solomon et al. (9) found that:
- 62% of the breast cancer patients who were appropriate for hereditary cancer risk assessment would have been missed due to incomplete cancer family history.
- 67% of colon cancer patients would have been missed due to incomplete cancer family history.
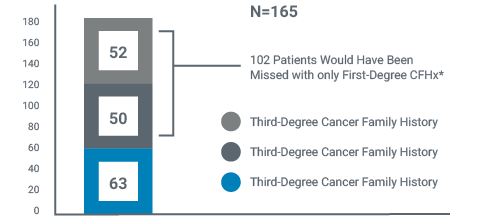
By focusing just on the breast cancer cohort, which consisted of 282 patients, it was observed that: (10)
- 63 patients were identified for hereditary cancer risk assessment based on first-degree family history
- By extending to the second degree, an additional 50 patients were identified
- By capturing third-generation, which is what NCCN recommends be included as part of a complete CFHx, an additional 52 patients were identified
By limiting the cancer family history to first-degree alone, 102 patients would have been missed for hereditary cancer risk assessment. This illustrates the fact that first-degree family history alone is not adequate for identification of all patients at risk for hereditary breast and colon cancer syndromes.
Patients at risk for Hereditary Cancer Missed When Using Only First-Degree Family History(3)

Additional Breast Cancer Patients Identified for Hereditary Cancer Risk Assessment When Using Multiple Degrees of Family History.
For a number of years, the National Comprehensive Cancer Network (NCCN) has authored guidelines to help providers assess patients for hereditary cancer risk and make the appropriate recommendations for further genetic testing. As a provider, some things to be aware of are multiple cancers in a patient, a particularly young cancer diagnosis, and rare cancers such as ovarian cancer, triple-negative breast cancer or male breast cancer.
Featured below are three case studies to further your knowledge around patients appropriate for further genetic testing.
Patient Diagnosed with Multiple Cancers
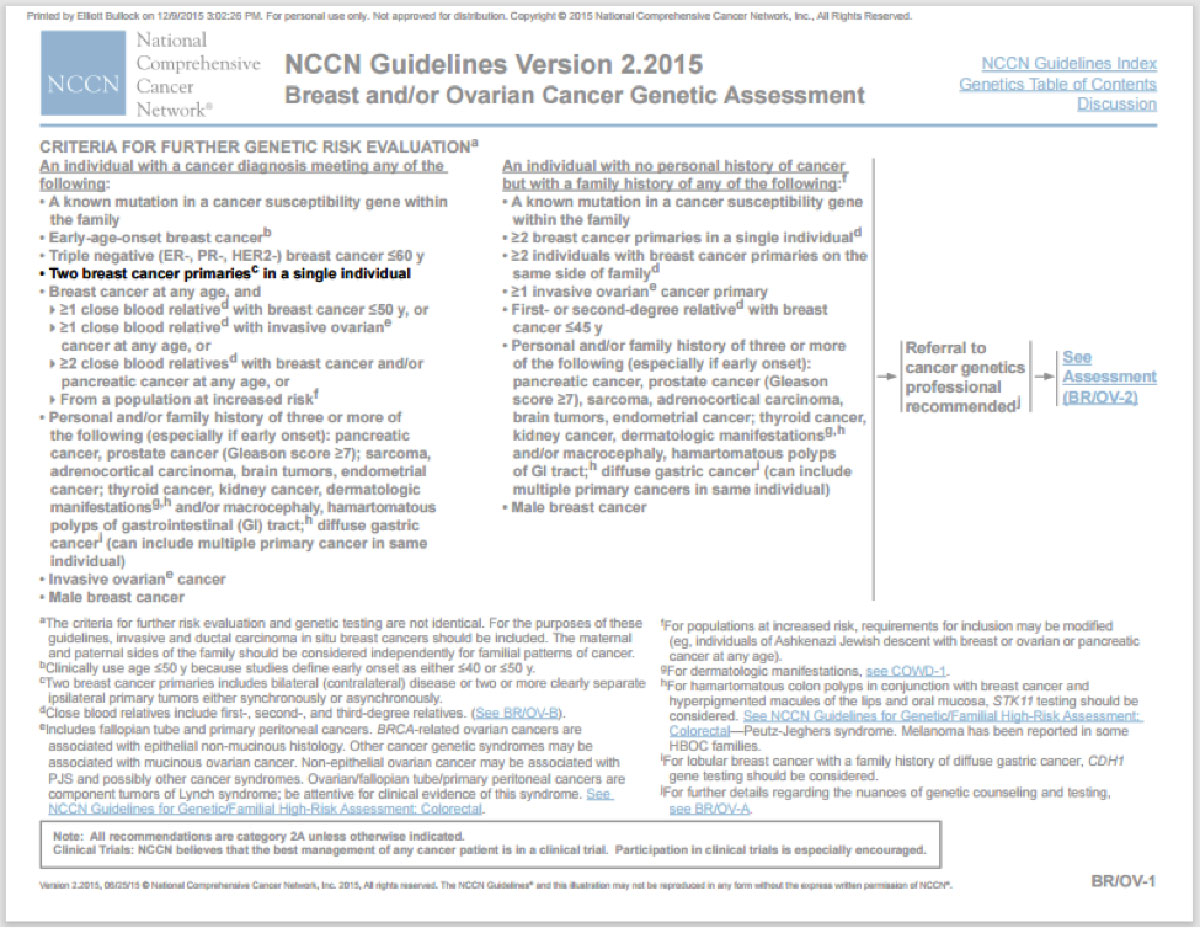
A 49 year old woman presents with Stage II breast cancer 2 years after a first diagnosis of breast cancer. Based on this patient’s multiple cancers, she is appropriate for further genetic testing. According to NCCN Guidelines for Detection, Prevention, and Risk Reduction, this patient meets the following guideline: (11)
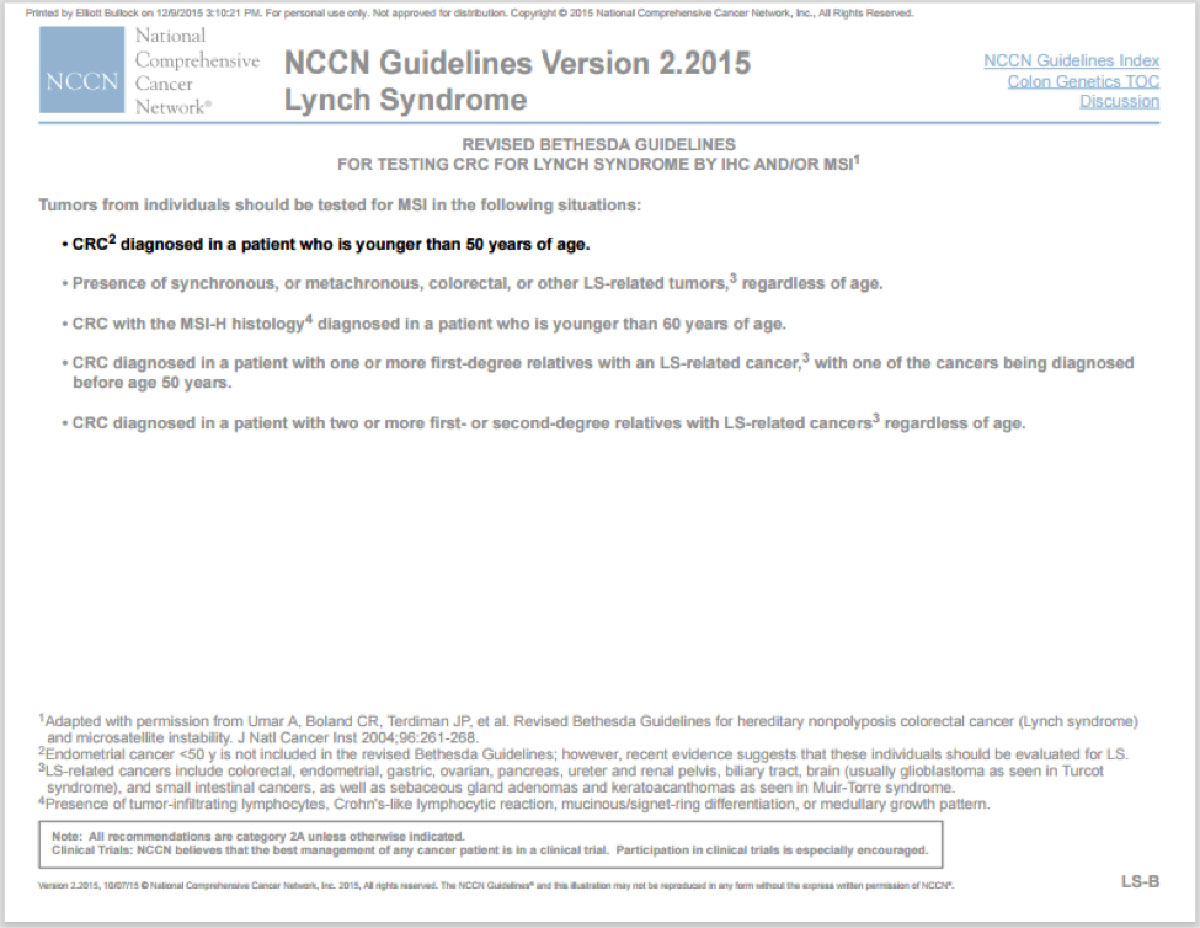
Patient with colorectal cancer diagnosed <50
A 42 year old male presents with Stage III colon cancer. Based on this early onset of cancer, this patient meets revised Bethesda criteria and is appropriate for further genetic testing. According to NCCN Guidelines for Detection, Prevention, and Risk Reduction, this patient meets the following guideline: (12)
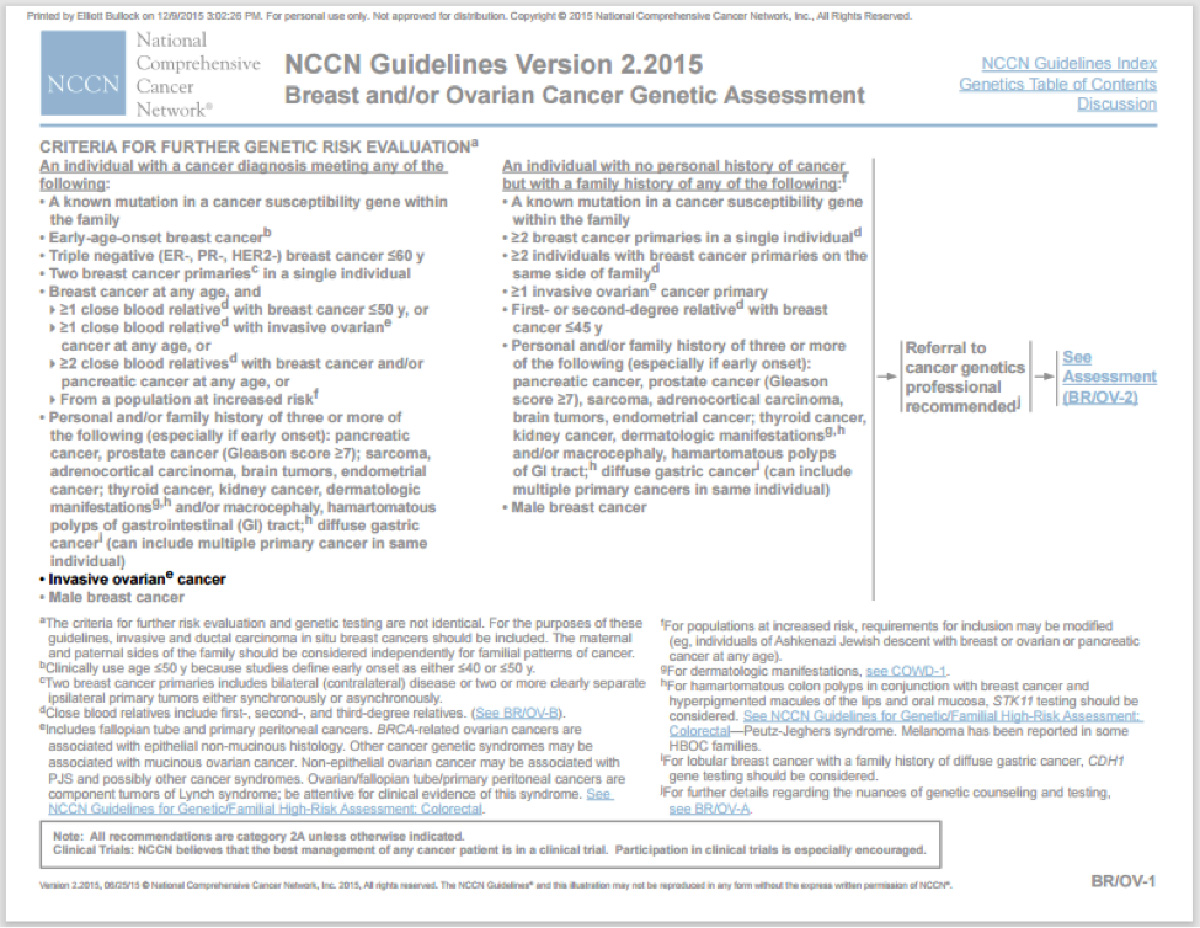
Patient Diagnosed with Ovarian Cancer
A 68-year-old women presents with ovarian cancer. Based on this rare diagnosis, this patient is appropriate for further genetic testing. According to NCCN Guidelines for Detection, Prevention, and Risk Reduction, this patient meets the following guideline: (13)
Based on the case studies above, it is important to evaluate these patients based on their personal history. ASCO recommends evaluating two generation CFHx that includes type of primary cancer, age at cancer diagnosis, as well as ethnicity(14) and NCCN recommends reaching out to third degree relatives to gather a complete CFHx.(15)
The four cases below illustrate the importance of a patient’s cancer family history when making further genetic testing determinations. (16)
Case Study 1: Breast Cancer
A 51 year old female presents with breast cancer. Her first- generation family history shows that her father was diagnosed with prostate cancer at age 63. Based on this information, this patient does not meet NCCN clinical criteria for hereditary cancer testing.
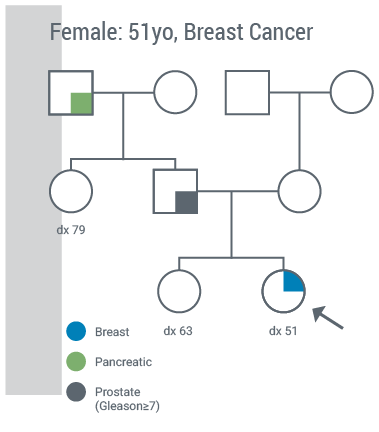
However, by expanding documented CFHx to the second generation, it is discovered that her paternal grandfather was diagnosed with pancreatic cancer at age 79.
With this documented second-degree family history information, she meets NCCN clinical testing criteria.
The guideline she meets is:
- Personal history of breast cancer diagnosed at any age with ≥2 close blood relatives with pancreatic and/or prostate cancer at any age.
Furthermore, if this patient is tested and found to carry a BRCA1 or BRCA2 mutation, there are potential management changes that will be made.
For example, a risk-reducing mastectomy over lumpectomy may be discussed as part of her treatment and a risk-reducing bilateral salpingo-oophorectomy (BSO) may also be recommended. If breast-sparing surgery is performed, the provider will likely recommend chemoprevention options to reduce the risk of a second breast cancer. In addition, they would likely recommend increasing breast surveillance.
Case Study 2: Ovarian Cancer
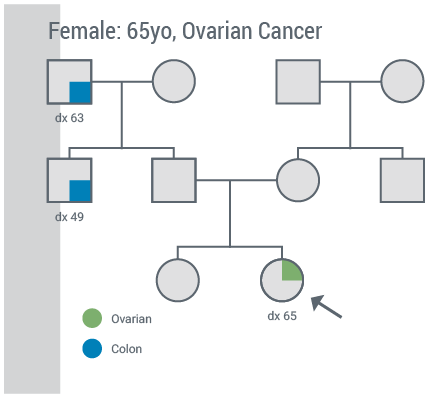
In this second case, a 65 year old presents with ovarian cancer. Based on her ovarian cancer diagnosis alone, this patient meets NCCN HBOC clinical testing criteria.
However, by capturing her second-degree family history, as should be done with all patients according to ASCO, it was determined that she has a paternal uncle who was diagnosed with colon cancer at the age of 49 and a paternal grandfather who was diagnosed with colon cancer at the age of 63.
With this documented second-degree family history information, this patient may be at risk for Lynch syndrome. The specific guideline this patient meets is
- Meets revised Betheseda Guidelines or Amsterdam Criteria
Furthermore, if this patient is tested and found to carry a Lynch syndrome mutation, there are potential management changes that should be considered.
For example, annual colonoscopies may be recommended as well as a consideration for prophylactic removal of her uterus to mitigate her risk of endometrial cancer in addition to a BSO to reduce her risk of ovarian cancer.
Case 3: Colon Cancer
A 58 year old male presents with colon cancer. Based on his documented first-degree family history, his father was diagnosed with thyroid cancer at the age of 62, but there is nothing to warrant additional screening for hereditary risk assessment.
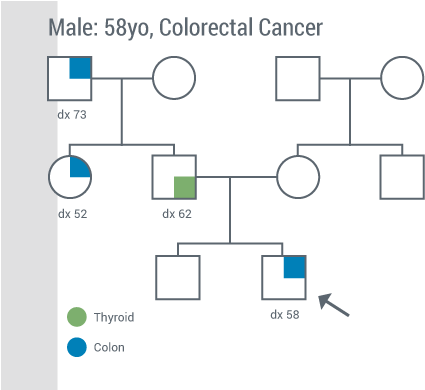
However, when a second-degree family history was obtained and documented, as recommended by ASCO, it is now known that his paternal uncle had colon cancer at the age of 52 and his paternal grandfather was diagnosed with colon cancer at the age of 73. With this new information, this patient is eligible for genetic testing as he meets revised Bethesda criteria for Lynch syndrome.
The specific guideline this patient meets is: an individual diagnosed with colorectal cancer and colorectal cancer diagnosed in 2 or more first- or second- degree relatives with HNPCC-related tumors regardless of age.
Now, if this patient is found to carry a Lynch syndrome mutation, there are some potential changes to his management that would be considered. For example, colonoscopies every 1-2 years for life post-treatment would be recommended according to NCCN guidelines.
CASE 4 (Endometrial Cancer):
A 62 year old female presents with endometrial cancer.
NCCN has added a new tool to help facilitate the identification of patients with Lynch syndrome - the PREMM model, which was developed by Dana Farber. Since we know that Lynch syndrome is composed of multiple types of cancers, this tool can help healthcare providers determine if patients meet NCCN criteria for testing. NCCN clinical testing criteria for Lynch syndrome states that once you input your patients’ personal and family cancer history into the PREMM model, if the prevalence is ≥5%, the patient is appropriate for Lynch syndrome testing.
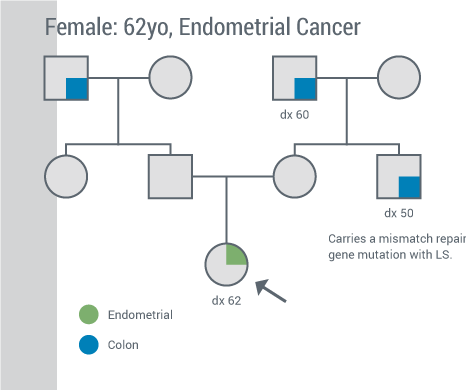
This patient that we discussed does meet clinical genetic testing criteria based on her ≥5% risk threshold according to the PREMM model. All patients with endometrial cancer have a >5% risk threshold according to the PREMM model.
Additionally, by obtaining her second-degree family history, as recommended by ASCO, it is determined that her maternal uncle was diagnosed with colon cancer at the age of 50 and carries a mismatch repair gene mutation associated with Lynch syndrome. This information would never have been captured had the patient’s complete family history not been taken.
Now, she meets guidelines for single site testing based on the previously identified mutation in the family.
If she is found to carry the mismatch repair gene mutation her uncle does, there are some potential management changes that her provider may suggest. For instance, prophylactic hysterectomy and BSO, CA-125 screening, and an increase in colonoscopy frequency to every 1-2 years may be recommended.
Copyright © 2015 Myriad Genetic Laboratories all rights reserved